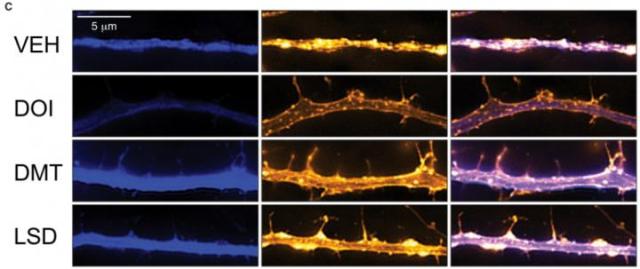
This figure shows the effects of three psychedelics and one control (VEH) on cortical neurons.
… A new study, published June 12 in the journal Cell Reports, found psychedelics, specifically DOI, DMT, and LSD, can change brain cells in rats and flies, making neurons more likely to branch out and connect with one another. The work supports the theory that psychedelics could help to fight depression, anxiety, addiction, and post-traumatic stress disorder.
… “One of the hallmarks of depression is that the neurites in the prefrontal cortex — a key brain region that regulates emotion, mood, and anxiety — those neurites tend to shrivel up,” says Olson. These brain changes also appear in cases of anxiety, addiction, and post-traumatic stress disorder. __
https://eurekalert.org/pub_releases/2018-06/cp-pdp060718.php
Psychedelics are not the most popular drugs for treating depression, but as we better understand how they promote the growth of new dendrites and synapses, we should be better able to develop safer and more effective antidepressants to accomplish the same effect.
More from Cell 12 June 2018:
Neuropsychiatric diseases, including mood and anxiety disorders, are some of the leading causes of disability worldwide and place an enormous economic burden on society (Gustavsson et al., 2011, Whiteford et al., 2013). Approximately one-third of patients will not respond to current antidepressant drugs, and those who do will usually require at least 2–4 weeks of treatment before they experience any beneficial effects (Rush et al., 2006). Depression, post-traumatic stress disorder (PTSD), and addiction share common neural circuitry (Arnsten, 2009, Russo et al., 2009, Peters et al., 2010, Russo and Nestler, 2013) and have high comorbidity (Kelly and Daley, 2013).
… Atrophy of neurons in the prefrontal cortex (PFC) plays a key role in the pathophysiology of depression and related disorders. The ability to promote both structural and functional plasticity in the PFC has been hypothesized to underlie the fast-acting antidepressant properties of the dissociative anesthetic ketamine. Here, we report that, like ketamine, serotonergic psychedelics are capable of robustly increasing neuritogenesis and/or spinogenesis both in vitro and in vivo. These changes in neuronal structure are accompanied by increased synapse number and function, as measured by fluorescence microscopy and electrophysiology. The structural changes induced by psychedelics appear to result from stimulation of the TrkB, mTOR, and 5-HT2A signaling pathways and could possibly explain the clinical effectiveness of these compounds. Our results underscore the therapeutic potential of psychedelics and, importantly, identify several lead scaffolds for medicinal chemistry efforts focused on developing plasticity-promoting compounds as safe, effective, and fast-acting treatments for depression and related disorders.
__ Psychedelics Promote Structural and Functional Neural Plasticity https://www.cell.com/cell-reports/fulltext/S2211-1247(18)30755-1
The neuroplasticity described in the 12 June 2018 paper in Cell consists of “neuritogenesis,” or the growth of dendrites and synaptic buttons — providing a denser connectivity between neurons.
Another form of neuroplasticity which may take place under some conditions is “neurogenesis,” or the growth of stem cells which develop into neurons. In adults, this may occur in the hippocampus and along the ventricular lining of the brain.
The hippocampus is the region of the medial temporal lobes thought to play a prominent role in the retention of long term memories. More on hippocampal (DG: dentate gyrus) neurogenesis:
… Here we assessed whole autopsy hippocampi from healthy human individuals ranging from 14 to 79 years of age. We found similar numbers of intermediate neural progenitors and thousands of immature neurons in the DG, comparable numbers of glia and mature granule neurons, and equivalent DG volume across ages. Nevertheless, older individuals have less angiogenesis and neuroplasticity and a smaller quiescent progenitor pool in anterior-mid DG, with no changes in posterior DG. Thus, healthy older subjects without cognitive impairment, neuropsychiatric disease, or treatment display preserved neurogenesis. __ https://www.cell.com/cell-stem-cell/fulltext/S1934-5909(18)30121-8
It is possible that some psychedelic mixtures may stimulate the transition of neural stem cells into functioning neurons:
When grown with ayahuasca compounds, the stem cells in the neurospheres also began to differentiate (change their properties) to resemble neurons more effectively than under control conditions. This means that the stem cells started to lose their stem-cell-like properties, and started making proteins that are found in adult neurons.
Overall, it seems that exposing neural stem cells to harmine, THH, and harmaline encourages them to grow and change into new neurons more effectively than under control conditions.
__ https://thepsychedelicscientist.com/2018/04/15/ayahuasca-neurogenesis/
This is All Very Controversial
Many neuroscientists still doubt that adult human brains can generate new neurons past adolescence. Proving that psychedelics can promote the growth of new neurons in the brain (eg hippocampus) will take some time, and perhaps a somewhat different perspective on neuropharmaceutical ethics than is dominant at this time.
It is less controversial to pursue the use of ketamine derivatives to promote new “branching” of existing neurons. But ketamine does not seem to be as effective at neuritogenesis as LSD, DMT, or psilocybin. In other words, some old prejudices may need to fall in order to achieve a better solution to an age-old scourge of the human spirit.
Here at the Al Fin Institutes of Neuroscience, we prefer the use of occasional treatments for chronic ailments over the everyday medication of persons. As people age, their ailments may tend to accumulate — as do the number of treatments required. Many persons may take as many as 10 to 20 medication doses per day. The use of psychedelics or psychedelic analogs for treating depression would likely be of an intermittent nature, rather than daily, and would help to cut down on the total daily dosage regimen.
We Actually Prefer to Avoid Medication Altogether
If possible, the avoidance of pharmaceuticals is best. Electromagnetic or photic approaches to treating depression are preferred, as are other alternatives such as advanced neurofeedback, mindfulness, and cognitive behavioural therapies.
Still, some people have experienced relief from depression lasting 6 months or longer from a single psychedelic experience, if well designed and overseen.
We have barely begun to understand all the productive approaches to functional neuroplasticity in the treatment of neurologic and neuropsychiatric disorders.
Renewed scientific interest in the use of psychedelics to treat disorders of the spirit can be seen as a positive sign.

Even though I only used one a few times in high school (psilocybin mushrooms) and would not do them today, I also believe that the psychedelics (sometimes called hallucinogens) have therapeutic value and should be both legalized and studied.
The human brain is capable of a great deal more than our dumbed-down cultures train us for.
Early brain development appears to provide critical developmental windows of exceptional neuroplasticity for different types of learning, at different stages of childhood. Most of our upbringings did not take advantage of all of those opportunities. But now we are beginning to discover ways of re-opening these critical windows of neuroplasticity for some types of learning.
Such areas of research are crucial for optimising a human future, even if they challenge old taboos.